Addressing Refugee Health Disparities: Exploring Refugee Health Programs at the University of Arizona
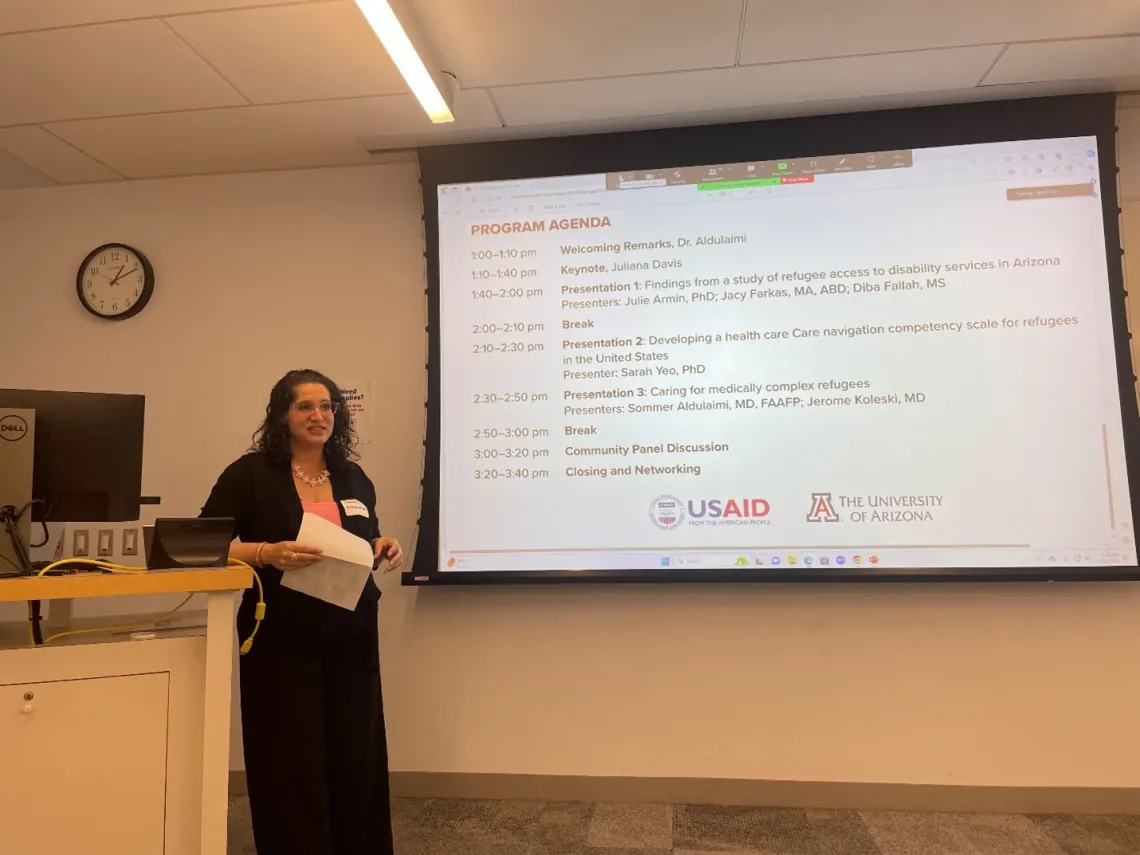
On January 31, several UArizona College of Medicine – Tucson Department of Family and Community Medicine faculty including Sommer Aldulaimi, MD, FAAFP, Julie Armin, PhD, Jacy Farkas, MA, ABD, and Jerome Koleski, MD, participated in Addressing Refugee Health Disparities: Exploring Refugee Health Programs at the University of Arizona, an inaugural conference dedicated to improving the resources available for refugees in Arizona. In addition to Family and Community Medicine and the Sonoran Center for Excellence in Disabilities, which also served on the planning committee for the conference, several organizations had representatives at the event, including the Amani Center, and International Rescue Committee, among others. The event was made possible through USAID.
“This event was meant to bring together various stakeholders, healthcare providers, researchers and community agencies who are invested in the well-being of refugees and to create an area for us to be able to talk to each other and network, and to learn about what's going on in the community and in and at the University of Arizona,” said Dr. Aldulaimi (pictured above), co-director of Global Health Programs and co-investigator for the Sonoran Center's refugee project, in the event’s opening remarks.
The event began in earnest with keynote speaker Juliana Davis. Davis is the State Refugee Health Manager at the Arizona Refugee Resettlement Program in the Department of Economic Security. She noted that refugees have their own unique supports to help them start their new life in the U.S., such as, “refugee cash assistance, refugee medical assistance, and a Temporary 12-month Transitional health coverage for refugees who fall off access due to income from employment.” They also receive a medical screening upon arrival, and it is here where the health disparities in refugee communities first become clear. In total, about 15% of the world's displaced peoples have a condition that qualifies as a disability. They may also have difficulties accessing healthcare due to linguistic and cultural barriers in addition to the complex nature of the U.S. healthcare system.
It is against this background that Davis showed some of the ways that support organizations have been making progress towards reducing these disparities and moving towards health equity, like videos about vaccinations in refugee’s native languages.
“This showed us two things in the long term: the medical community needed to increase their cultural knowledge, cultural safety and cultural humility; and we needed to invest in community health worker methods with refugees,” Davis said.
With this example in mind, the other speakers at the conference detailed the ways in which their organizations were contributing to this larger goal.
Following Davis’ keynote, the Sonoran Center’s Jacy Farkas and Dr. Julie Armin, along with Diversity Fellow and graduate research assistant Diba Fallah, presented on their project titled “Elevating Refugee Perspectives About Access to Disability Services in Arizona,” which combined survey, qualitative research, and data analysis to determine the accessibility of services to refugees with disabilities, as well as areas where improvement is possible.
“Our project goals were to understand access to, and use of, disability services for the diverse communities of refugees with disabilities and to describe best practices, reduce gaps and increase access to disability services for refugees with disabilities,” said Fallah.
First, the project team set about gathering data. “[We fostered] community engagement through a reciprocity approach. A part of that was forming a Community Advisory Board who came from refugee organizations, disability organizations and public schools, and they shared input on data collection data, interpretation, and recommendations,” Fallah explained.
Fallah then explained how they used Group Concept Mapping—a method that enables researchers to work with communities to identify and achieve consensus on community priorities—to determine which statements are most important.
“We selected a handful [of important statements]: getting timely diagnoses, having case managers who really specialize in refugee care, and of course interpretation available through those systems,” she continued.
This data collection was complemented by a thorough review of current Arizona law, policy, and practice relating to services for refugees with disabilities. The team also conducted a series of in-depth interviews with refugee communities to corroborate and evaluate their findings.
After a short break, the conference reconvened for a presentation given by Sarah Yeo, PhD, a postdoctoral researcher and lead organizer at the University of Arizona Cancer Center and co-founder of the conference. Dr. Yeo’s presentation centered on developing a health care navigation competency scale for refugees in the U.S.
“I started this project to identify the core competencies that are required by refugees to navigate the complex U.S. healthcare system, so that they [refugee resettlement agencies] can measure the actual level of competencies and provide more for the most vulnerable who are suffering the most,” Dr. Yeo said. “There are few tools to measure health competency, and many of them are based on the assumption that the participants speak English as a mother tongue. It is inadequate for those populations such as refugees who speak English as their second language or who do not speak any English.”
Based on interviews with patients and experts, Dr. Yeo created a scale that measures several aspects of health navigation, including health system knowledge, insurance, making appointments, transportation, preparing for visits, interpretation, medicine, medical bills, preventative care, and more.
Dr. Yeo hopes to conduct a cross-representational survey to validate the scale and measure the spread of chronic diseases and identify risk factors for such conditions.
The final presentation, given by co-directors of Global Health Programs Dr. Sommer Aldulaimi and Dr. Jerome Koleski, focused on the needs of caring for medically complex refugees. Drs. Aldulaimi and Koleski run a complex care refugee clinic. In this context, ‘medically complex’ means someone with “a physical or mental abnormality, disease, or disability, serious in degree or nature amounting to a substantial departure from well-being.”
The pair first detailed some of the prevalent conditions among refugee communities that contribute to medical complexity. They then explained some of the barriers to care, including language, cultural differences, trust in provision of care, short appointment times, discrimination both in their home countries and in the U.S., high costs, bureaucratic red tape, poor housing and lack of information on health resources.
In the work at their clinic, they have identified some strategies for navigating these barriers for individuals. These include appropriate language interpretation, a safe and caring patient-physician relationship, allowing patients to discuss trauma without interruption, and avoiding labels and rushing to diagnoses.
Thinking about how these strategies map to the level of policy, Drs. Koleski and Aldulaimi created another list of strategies: multidisciplinary work, universal health care for refugees, online resources for primary care providers and refugees, skill development for those caring for refugees, coordination and integration of care, increased funding for resettlement and service agencies, and general advocacy.
Finally, the conference concluded with a panel discussion with refugee-serving community organizations. The panel members were (pictured below, left to right) Amelia Natoli with Iskashitaa Refugee Network, Sophie Herran with Jewish Family & Children's Services of Southern Arizona, Linda Kraemer of the International Rescue Committee, and Sahra Hirsi with the Amani Community Center.

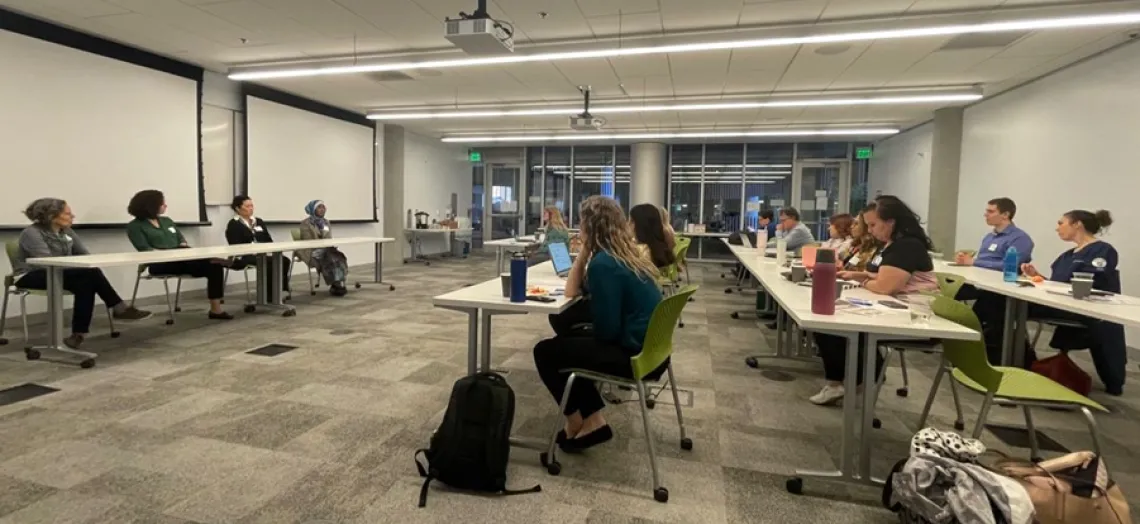
The panelists began by covering upcoming developments that they were excited about. Herran’s organization will begin offering a therapy and healthcare navigation program for Afghan refugees impacted by combat. Kraemer also discussed how refugee resettlement organizations are building capacity for refugees to gain job skills and training by offering English language training and career guidance programs. An audience member mentioned that they are working in a program that works with high-school aged refugees and brought up the possibility of a collaboration between their agencies.
Ultimately, the conference was an excellent opportunity for sharing resources, networking, and collaboration among organizations serving refugees in Arizona. Given the success of this year’s conference, the Sonoran Center and its partners are looking forward to collaborating on the conference again in the years to come.
